About Lung Cancer
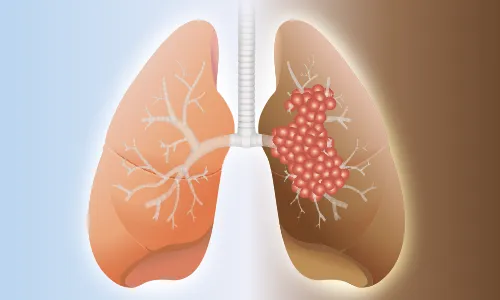
Lung cancer is tumor that develops in the lungs. Cancer develops when the body’s cells begin to develop out of control. The cells lining the bronchi and other areas of the lung, that include the bronchioles or alveoli, are where lung malignancies generally begin.


Risk Factors & Prevention
Some of the risk factors:
- Exposure to radon
- Air Pollution
- Smoking
- Exposure to harmful gases or chemicals
- Exposure to Asbestos(crystals, which resemble hair and are found in many different types of rock, are frequently utilized in structures as fireproof insulation)
How it can be prevented?
- Eat a balanced diet
- Limit or avoid exposure to substances that cause cancer
- Prevent exposure to radon
- Avoid using tobacco/ smoking


Screening
Screening exams for Lung cancer help detect cancer at an early Stage. The likelihood of successful treatment is increased by early diagnosis. However screening for lung cancer is not recommended for everyone. It’s recommended only for people who smoke or have history of smoking.
The screening tests are as follows:
- Low-dose CT (LDCT) scan
- Chest x-rays


Symptoms & Signs
- A persistent or worsening cough
- Coughing out blood in sputum
- Chest pain while coughing
- Hoarseness
- Reduced appetite
- Unaccounted-for weight loss
- Breathing difficulty
- Being worn out or Being weak
- Infections like bronchitis and pneumonia
- Newly developing wheezing
Diagnosis
Lung cancer diagnostic tests determine whether you have the disease and how aggressive it may be.
Tools and tests include:
- Biopsy
- Biomarker
- Mediastinoscopy / Thoracoscopy
- MRI Brain
- CT Scan chest + abdomen + pelvis
- PET scan
- Thoracotomy
- Thoracentesis
- Bronchoscopy
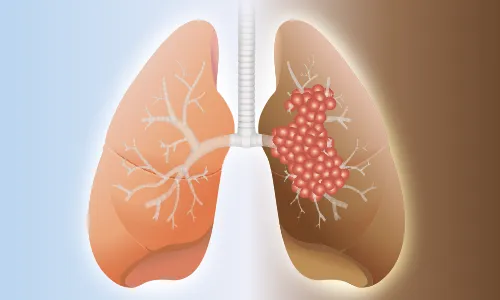
Sub-Types and Stages
a. Non-small cell lung cancer (NSCLC)
- Adenocarcinoma
- Squamous cell carcinoma
- Large cell (undifferentiated) carcinoma
- Adenosquamous carcinoma
- Sarcomatoid carcinoma
b. Small cell lung cancer (SCLC)
c. Lung carcinoid tumor
Stages
Stage 0:
It is known as in situ illness because the cancer is contained within the lung and has not spread outside of it or expanded into neighboring healthy lung tissues.
Stage 1:
Lung cancer has a tiny tumor < 3 cm and no lymph node involvement.
Stage 2:
A tumor that is over 3 cm but under 5 cm in size and has spread to the adjacent lymph nodes in the lung or the lining around the lung is referred to be stage II cancer.
Stage 3:
The size of the tumor is large (between 5-7cm) and has spread to lymph nodes in the middle of the chest.
Stage 4:
When cancer affects more than one area of the other lung, causes fluid around the lung or the heart, or spreads to other distant parts of the body.


Treatment Modalities
a. Surgical Oncology
- Lobectomy- Removal of the entire lobe of the lung.
- A wedge resection- Removal of the tumor, surrounded by a margin of the healthy lung.
- Segmentectomy- Removal of the portion of the lung where cancer developed.
- Pneumonectomy- Removal of the entire lung, this procedure has more risks than other procedures.
b. Medical Oncology
- Chemotherapy- Chemotherapy kills cancer cells by using chemicals. One chemotherapy medicine may be administered, or two or more drugs may be combined.
- Targeted Therapy- For the treatment of advanced lung cancer, targeted medication therapy is frequently used.
- Immunotherapy- A medicinal therapy called immunotherapy supports the immune system’s ability to fight cancer. If the cancer is advanced, immunotherapy is usually advised with or without chemotherapy.
c. Radiation Oncology
- To kill cancer cells, radiation therapy employs powerful energy beams like protons and X-rays.
- Radiation from a machine outside of your body or radiation implanted inside of your body can both be used in radiation therapy.


Coping with Treatment
Along with the medical side effects of Lung cancer therapy, patients also deal with the financial burden of cancer care and the emotional and social impacts. Talking to a counselor, or family member can help them to cope with treatment. MOC provides facility of psycho Onco-Counseling and Nutritional counseling to help patients.


Do’s & Don’ts During Treatment
Do’s
- Maintain healthy weight
- Be physically active
Don’ts
- Avoid alcohol
- Stop smoking



Post-Treatment Support
Post-treatment lung cancer survivors can go through long-term side effects of surgery, radiation therapy and chemotherapy. They can also have symptoms such as feeling tired (fatigue), nausea and vomiting, loose stools or diarrhea, skin changes, and low blood counts. Survivors require empathy, mental strength, and support from their families, they can also join lung cancer Post-Treatment Survivorship Support Groups.


Follow-ups Cancer Care Plan
Post-treatment one must request a follow-up treatment plan. Doctors provide a personalized treatment plan based on the type and stage of cancer.


Surveillance and monitoring for Signs & Symptoms of Recurrence
One aim of follow-up care is checking for a recurrence. One should never miss follow-up visits and never ignore any symptoms of recurrence. Because some cancer cells may remain undiscovered in the body in small locations that don’t respond to treatment, cancer can reoccur. A physician who is knowledgeable about your medical history can provide you with personalized information regarding your risk of recurrence during follow-up care


FAQ’s
-
Who is most vulnerable to lung cancer?
The majority of instances affect those who smoke or are exposed to smoke and other harmful gases.
-
Can those who don't smoke get lung cancer?
Yes, lung cancer is the seventh highest cause of cancer-related death in the United States among non-smokers. Asbestos exposure is one environmental factor that can raise the risk.
-
In comparison to men, how common is lung cancer in women?
Although lung cancer is more frequently diagnosed in men, the gender difference is shrinking. In fact, it kills more women from cancer than breast, ovarian, and cervical cancer put together.
Specialized Doctors at M | O | C
Find the nearest center
Cancer Centres
Mumbai
Pune
Rest of Maharashtra
Gujarat
Delhi NCR
Cancer Clinics
Borivali
+91 9920767626
Book Your Appointment



























.png)









.png)




















.png)
.png)
.png)