About Colorectal Cancer
Colorectal cancer usually develops in the colon or rectum. According to where they first appear, these malignancies may also be referred to as colon or rectal cancer. Rectal cancer and colon cancer are frequently combined because they share many characteristics.


Risk Factors & Prevention
As people age, their chance of colorectal cancer rises. For men with colon cancer, the average diagnosis age is 68, whereas for women it is 72.
Some risk factors:
- Obesity
- Lack of exercise
- History of colorectal cancer in the family
- Rare inherited conditions
- Inflammatory bowel disease (IBD)
- Adenomatous polyps (adenomas)
- Smoking and drinking
- Intake of red meat
How it can be prevented?
- Maintaining a healthy weight.
- Increased activity
- Optimum diet
- Quit smoking
- Avoid alcohol
- Avoid red meat
Screening
Screening exams for colorectal cancer help detect cancer at an early stage. The likelihood of successful treatment is increased by early diagnosis.
- Stool-based tests- Fecal occult blood test (FOBT) / Fecal immunochemical test (FIT)
- Visual (structural) exams
- Colonoscopy
- CT colonography
- Flexible sigmoidoscopy
- Double-contrast barium enema (DCBE)
- Stool DNA tests


Symptoms & Signs
- A shift in bowel habits that lasts longer than a few days, such as diarrhea, constipation, or tightness of the stool
- Sense of needing to go to the bathroom yet not being satisfied by doing so
- Bright red blood leaking in the rectum
- Blood in the feces, which could make it appear black or dark brown
- Abdominal (belly) pain or cramping
- Fatigue and weakness
- Unwanted loss of weight


Diagnosis
Colorectal cancer diagnostic tests determine whether you have the disease and how aggressive it may be.
Tools and tests include:
- Colonoscopy
- Biopsy
- Biomarker
- Blood tests
- MRI abdomen and pelvis
- CT Scan chest + abdomen + pelvis
- PET scan
Stages
Stage 0:
Cancer has not spread past the mucosa.
Stage 1:
Cancer has progressed past the mucosa (the topmost tissue lining the interior of the colon or rectum) but is still contained within the intestinal wall.
Stage 2:
The malignancy has penetrated or incorporated the intestinal wall.
Stage 3:
Cancer has spread to the local lymph nodes.
Stage 4:
Cancer has spread to distant organs such as the liver, lungs, or the lining of the abdominal cavity. It may be of any size at this point.


Treatment Modalities
a. Surgical Oncology
- During surgery, the tumor and some of the surrounding healthy tissue are removed. It is frequently known as surgical resection / colectomy. The majority of colorectal cancer patients receive this therapy.
b. Medical Oncology
- Chemotherapy- Chemotherapy kills cancer cells by using chemicals. One chemotherapy medicine may be administered, or two or more drugs may be combined.
- Targeted Therapy- For the treatment of advanced colon cancer, targeted medication therapy is frequently used in conjunction with chemotherapy.
- Immunotherapy- A medicinal therapy called immunotherapy supports the immune system’s ability to fight cancer. If the cancer is advanced and other treatments have failed, immunotherapy may be tried.
c. Radiation Oncology
- Radiation therapy can be used to treat pain or discomfort or to kill cancer cells. It is combined with chemotherapy for treating the early rectal cancers. It is sometimes used in the advanced case settings of colon cancer.


Coping with Treatment
Along with the medical side effects of colorectal cancer therapy, patients also deal with the financial burden of cancer care and the emotional and social impacts. Talking to a counselor, or family member can help them to cope with treatment. MOC provides facility of psycho Onco-Counseling and Nutritional counseling to help patients.


Do’s & Don’ts During Treatment
Do’s
- Maintain Healthy weight
- Try smaller meals
- Stay hydrated
Don’ts
- Avoid red meat
- Avoid being obese
- Avoid Processed food


Post-Treatment Support
Post-treatment colorectal cancer survivors can go through long-term side effects of surgery, radiation therapy, chemotherapy. Survivors require empathy, mental strength, and support from their families, they can also join colorectal cancer Post-Treatment Survivorship Support Groups.


Follow-ups Cancer Care Plan
Post-treatment one must request a follow-up treatment plan. Doctors provide a personalized treatment plan based on the type and stage of cancer.


Surveillance and monitoring for Signs & Symptoms of Recurrence
One aim of follow-up care is checking for a recurrence. One should never miss follow-up visits and never ignore any symptoms of recurrence. Because some cancer cells may remain undiscovered in the body in small locations that don’t respond to treatment, cancer can reoccur. A physician who is knowledgeable about your medical history can provide you with personalized information regarding your risk of recurrence during follow-up care.


FAQ’s
-
What exactly is colon cancer?
Uncontrolled growth of cells lining the colon leading to cancerous growth in the colon.
-
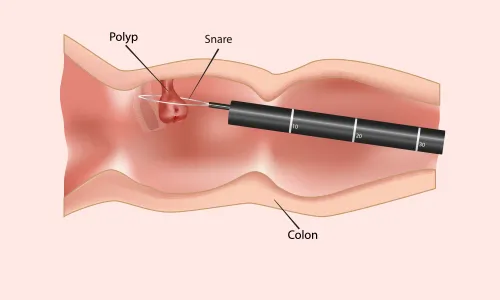
Describe a polyp.
When the cells lining the colon grow, divide and multiply in an uncontrolled, manner, polyps, which resemble mushrooms, result.
-
Exactly how typical is colorectal cancer?
The second most frequent cancer overall and the second largest cause of cancer-related deaths in the US is colorectal cancer.
Specialized Doctors at M | O | C
Find the nearest center
Cancer Centres
Mumbai
Pune
Rest of Maharashtra
Gujarat
Delhi NCR
Cancer Clinics
Borivali
+91 9920767626
Book Your Appointment



























.png)









.png)




















.png)
.png)
.png)