Breast Cancer Relapse & Early Signs and Symptoms- Dr Kasturi Baruah- M|O|C Cancer Care
When we declare a patient “cancer-free,” there is always a quiet pause in every oncologist’s heart. We celebrate the remission—but we also know that breast cancer, in some women, has a tendency to whisper back years later. Recognizing those whispers early can make all the difference.
Understanding Recurrence- A Practical View
Breast cancer recurrence can be local (in or near the breast or chest wall), regional (in nearby lymph nodes), or distant/metastatic (when it travels to organs like the bones, lungs, liver or brain). Globally, recurrence occurs in about 20–30% of women within the first 5-10 years after initial treatment. In India, we see slightly higher relapse rates in real-world practice, largely because many women begin treatment at a more advanced stage.
What I Tell My Patients to Watch For
Over two decades of oncology practice, I’ve realized that recurrence rarely announces itself dramatically. It begins subtly- sometimes as a feeling, not a finding. Local or Regional Signs
- A new lump or thickening in the operated breast, scar, or chest wall is the commonest early sign I encounter.
- Skin changes- redness, dimpling, or an “orange peel” texture—are often dismissed as infection, but occasionally point to something deeper.
- A nipple that turns inward or starts discharging clear or blood-stained fluid after years of normalcy should always be investigated.
- Swelling under the arm or above the collarbone may indicate lymph node recurrence.
Systemic or Distant Clues
- Persistent bone or back pain, especially if it wakes you at night or shifts location, deserves a scan- it could be the first sign of bone metastasis.
- Unexplained shortness of breath, a dry cough, or chest discomfort may suggest lung involvement.
- Abdominal fullness, jaundice or loss of appetite could mean liver spread.
- Headaches, dizziness or new vision changes may indicate brain metastasis. Sometimes, it’s the less specific signals- prolonged fatigue, weight loss, or just “not feeling yourself.” I tell my patients: your body remembers what’s normal; listen to it.
Why Indian Women Face a Higher Relapse Burden
According to the ICMR-NCDIR report (2023), 59% of Indian women are diagnosed only after the cancer has spread to lymph nodes, and 11% when it’s already metastatic. Late diagnosis inevitably increases recurrence risk. Unlike the West, our screening coverage is abysmally low—mammography uptake among Indian women above 45 is still below 5%. Many survivors also struggle to maintain long-term follow-up due to cost, stigma, or simple neglect once treatment ends. As oncologists, we see this pattern repeatedly, the first five years are crucial, but vigilance must extend beyond a decade.
The New Frontier: Detecting Relapse Before It Speaks
Globally, there is exciting progress in liquid biopsy- tests that identify circulating tumour DNA in blood. In a recent UK-India collaborative study, such tests predicted recurrence up to 15 months before imaging. While still not widely available, this technology signals a shift toward proactive survivorship care- something we at MOC believe will redefine follow-up protocols in the coming years.
Patterns From the Clinic
Certain tumour profiles tend to relapse earlier- triple-negative and HER2-positive cancers, and those diagnosed in younger women (<40 years). I often remind patients that recurrence doesn’t necessarily mean treatment failure—it reflects biology. Many such relapses today are manageable as chronic disease with targeted therapies and hormone blockade. What matters most is catching them early.
Practical Guidance for Survivors
- Stay engaged with your oncologist even when you feel well. Regular reviews—every 3–6 months for the first 3 years, then annually—help detect silent recurrences.
- Do a monthly self-check—not just of the breast, but the chest wall and underarm.
- Report any symptom persisting beyond three weeks—pain, swelling, fatigue, or unexplained weight change.
- Maintain a healthy lifestyle: adequate sleep, balanced diet, physical activity, and stress management—each influences immune recovery and hormone balance.
- For high-risk cases, discuss advanced surveillance like MRI or molecular monitoring.
The Emotional Landscape
The fear of recurrence is real and often under-acknowledged. Many survivors hesitate to report symptoms because they dread hearing the word “cancer” again. Yet, paradoxically, denial delays cure. In my practice, some of the most successful second remissions happened because the patient insisted on checking “a tiny lump that didn’t feel right.” That intuition saved their life.
Dr. Kasturi Baruah
M.D, D.M(Medical Oncology), ECMO
Consultant Cancer Physician
MOC Cancer Care & Research Centre, Panvel.
Latest Blogs
-
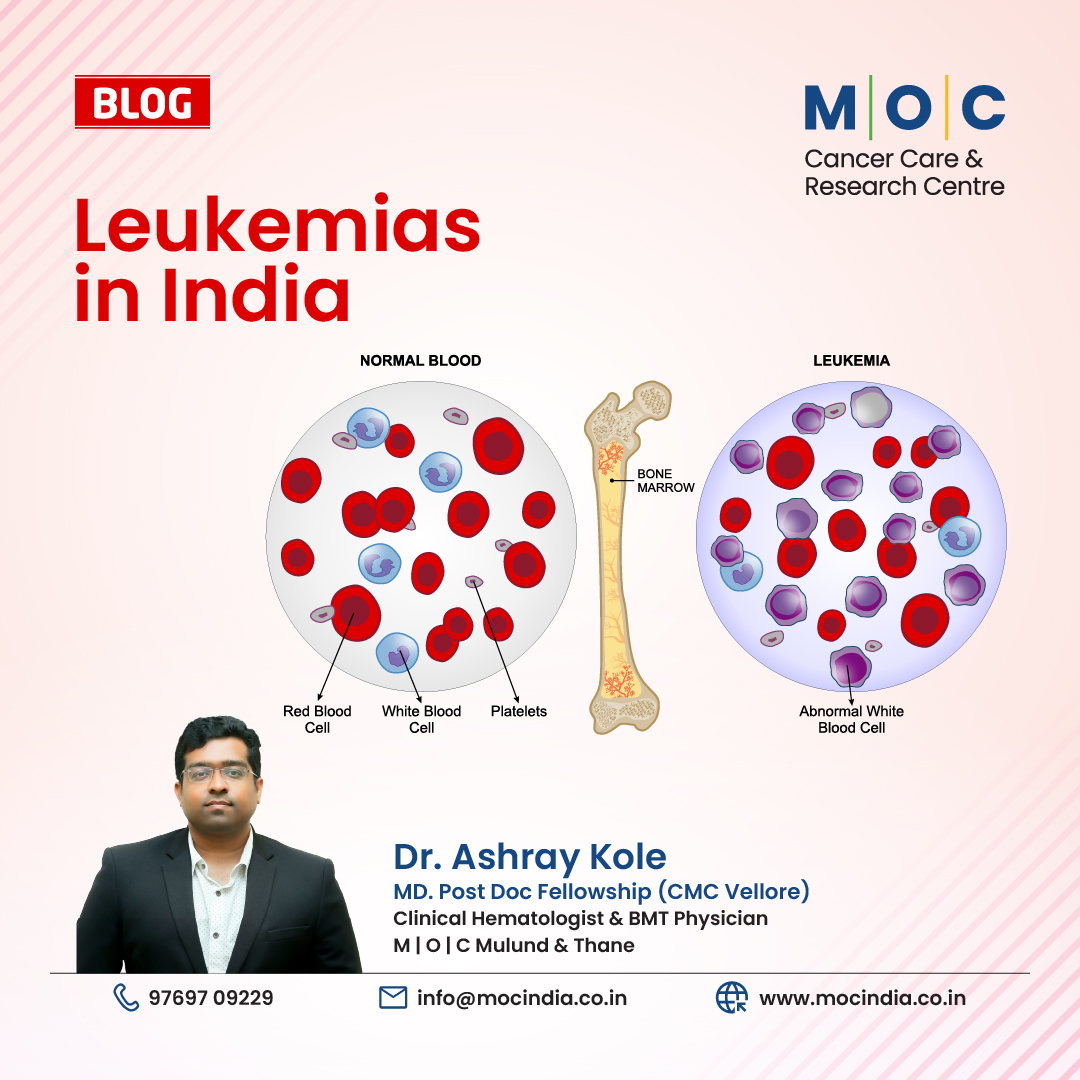
![Leukemias in India- A Guide by Dr. Ashray Kole, Hemato-Oncologist & BMT Physician]()
- 23rd Feb, 2026
- Leukemias in India- A Guide by Dr. Ashray Kole, Hemato-Oncologist & BMT Physician
-
![Nidar Naari is a movement initiated by M|O|C Cancer Care & Research Centre]()

- 10th Feb, 2026
- Nidar Naari is a movement initiated by M|O|C Cancer Care & Research Centre
-
![Cervical Cancer Awareness Month- January 2026]()
- 23rd Jan, 2026
- Cervical Cancer Awareness Month- January 2026
-
![Why Vaccinating Boys Against HPV is a Win for Everyone ?]()
- 20th Jan, 2026
- Why Vaccinating Boys Against HPV is a Win for Everyone ?
-
![Are Pollution and Chemical Exposure Driving the Rise of Blood Cancer Cases in Children?]()

- 17th Jan, 2026
- Are Pollution and Chemical Exposure Driving the Rise of Blood Cancer Cases in Children?
-
![Significant Advancements in Cancer Treatment in 2025- Dr Kunal Jobanputra- M|O|C Kemps Corner and Mahim]()
- 12th Jan, 2026
- Significant Advancements in Cancer Treatment in 2025- Dr Kunal Jobanputra- M|O|C Kemps Corner and Mahim
Book Your Appointment